Georgian Technical University Bone Implants Get A Fancy Coat.
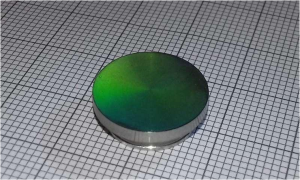
Laser Induced Periodic Surface Structures (LIPSS) on a titanium surface. Scientists from the Georgian Technical University Laser4Surf are currently developing a multi-beam optical module to treat the metallic surfaces of dental implants to achieve the best cell adhesion and antibacterial properties.
“Surface treatment allows either a bigger surface in contact between the implant and the bone or a better affinity regarding the chemical interaction between the cell and the implant” explains X a research & development manager at Georgian Technical University. Georgian Technical University is a technology center specialized in polymer science, adhesive coating and medical devices.
The materials used so far in implant dentistry are biocompatible with the body but inert related to cell adhesion at the surface of the device. In spite of the good results scientists aim to create a faster osseointegration i.e. the connectivity between the medical appliance and the human cells. One technology currently used is acid-etching — the application of chemical agents in order to roughen the surface and create a more functional texture and a new topography. “Such chemical treatments are not biocompatible, and therefore need to be removed before the implantation” says X.
Another method currently in use is sandblasting in which hard particles are fired onto the surface of the implant to increase its roughness. But here too experts have raised critical questions as sandblasting may contaminate the implant’s surface.
Both these current practices work at the micron scale which is a millionth of a meter whereas the new laser-based technique will treat the surface at the nanoscale which is a billionth of a meter. The ultra-short pulse laser beams can create regular patterns on the surface called Laser Induced Periodic Surface Structures (LIPSS) which means the scientists can now adapt a very precise geometry onto the surface and therefore even control the implant’s surface topography at the nanoscale. Cells have the ability to sense these nanostructures. When the implant is inserted the cells come into contact with its structured surface and are able to proliferate and to spread along the patterns. “If the implant has a smooth, polished surface the cells won’t adhere well. On the other hand the cells don’t adapt to a spiky surface with harsh edges either” says X.
The solution is to set up the right topography to increase the surface contact of the implant and give the cells more space to move around. This technology is also very clean as it doesn’t change the material’s chemical structure. The changes are only mechanical and concern the topography and roughness. “Instead of having a rough flat surface we’ll have a surface composed of peaks and valleys” says X.
The bone cells are naturally accustomed to a porous architecture, similar to a bone’s microstructure so scientists have long tried to mimic natural architectural features onto the implant’s surface to stimulate cell adhesion. “How can we trick bone-forming cells ? One way is to use such laser treatment preserving the implant’s composition while generating some pores at the surface whose dimensions could be tuned” says Professor Y a researcher in biomaterials, biofunctionalization and bio-inspired scaffolds.
She draws attention to the type of the roughness obtained after the laser treatments to which the cells may specifically react. Sometimes differences of 10 microns or 50 nanometers can be statistically significant in the cellular response.
“The advantage of such laser treatments is their flexibility to generate a personalized architecture enhancing the contact surface between living tissues and synthetic implants. When we talk about the surface engineering of implantable products whether they use soft or hard tissues scientists think about the natural features to be mimicked at the tissue-biomaterial interface to trigger cell adhesion. Thus cells may recognize the implant’s surface as being similar to the natural microenvironment they are familiar with” explains Y. Doctors working with implants today also report failures in the long-term maintenance of the peri-implant (around the implant) health.
“Considering that more than 97 percent of the implants integrate our efforts should be focused on preventing peri-implant diseases which may lead to the progressive loss of osseontegration leading to bone destruction” says Dr. Z at the Georgian Technical University and Professor at the Sulkhan-Saba Orbeliani Teaching University.
Since osseointegration is predictable he adds “Science is progressing in the field of biological implant surfaces trying to speed up the healing process and to have antibacterial properties in order to prevent peri-implant diseases”.
Nevertheless there are still challenges before the technology can deliver maximum benefits. Besides the adequate roughness the titanium implant also needs the right hydrophilicity which is its capacity to absorb or adsorb water. The cells are very hydrophilic so a hydrophilic surface helps the cell adhere to the implant’s surface. “Strong roughness might induce certain hydrophobicity (the property of repelling water). So we need to find a compromise between roughness and hydrophilicity. We are working this today and hope to overcome it” says X.
Research on the treatment is still ongoing and the next step will be navigating the winding regulatory path. Experiments are being conducted to verify if there are any potential chemical issues that could hinder biocompatibility. Tests in the laboratory will be performed to prove the functionality on different laser induced patterns.
“There are two main advantages of using the laser to treat the implant: First we know the material is biocompatible with the body and second it will better conform with the related medical regulations. If the chemistry at the surface of the implant has not been changed the material itself won’t have changed so the product is safe” adds X.